Conference Programme
2024 Programme Overview
The conference, in Telford in November 2024, featured keynote presentations, invited speakers, and free papers chosen from submitted abstracts. A third track featured insightful updates from industry partners on technology, products and software.
Our conference programme is always designed to ensure that you leave the event with insights that will help shape and inform your approach to clinical practice, research, and teaching.
This year’s event included keynote speakers, renowned experts, and industry pioneers who inspired and challenged delegates, with updates on quality improvement, engagement and service innovation, along with clinical practice and research.
As in previous years, we were delighted that our Official BAA Sponsors contributed to our programme with their own talks over the two days, details of which will be released in the Summer.
Here’s a summary of what we enjoyed in the 2024 programme:
- Dr Brent Edwards presented the Adrian Davis lecture. Dr Edwards is Director of the National Acoustic Laboratories, Australia – world leaders in hearing research. Dr Edwards spoke about Revolutionising Audiological Care Through Innovation in Clinical Tools and Treatment Strategies
- The Bamford lecture focused on a new era in the treatment of genetic hearing loss – genomic therapies, and was presented by Professor Manohar Bance, Professor of Otology and Skull Base Surgery, University of Cambridge
- Other keynote speakers included Rebecca Bennett, Senior Research Audiologist at the National Acoustic Laboratories who spoke about Managing the social and emotional wellbeing impacts of hearing loss: Interventions and approaches that can be implemented to augment current clinical practise, and a joint keynote from two main UK charities – NDCS and RNID. Dr Sam Lear and Crystal Rolfe joined forces to offer practical help for our workplaces around Deaf Awareness
- Invited speakers led thought-provoking parallel sessions, looking at all aspects of audiology across all sectors, from research to clinical practice.
- Research posters and oral presentations, submitted by you and fellow audiology professionals from across the UK
Presentations are all recorded, and delegates will receive a link to watch the presentations that we have permission to share.
2024 Speaker Abstracts and Biographies
Speaker Abstracts and Biographies:
Adrian Davis Lecture: Revolutionising Audiological Care Through Innovation in Clinical Tools and Treatment Strategies
Dr Brent Edwards, Director, National Acoustic Laboratories, Australia

Abstract
Hearing healthcare is evolving faster than it ever has. Innovation in technology is producing a wide array of choices for hearing care professionals to offer their clients, while a growing number of products are being developed for those with hearing difficulty to help themselves without the need of a hearing care professional. Apple, for example, have introduced a new category of hearing health technology through its AirPods Pro. Additionally, the rapid development of artificial intelligence (AI) innovation is changing all aspects of healthcare, and will have a dramatic impact on hearing healthcare services. All these changes present both challenges and opportunities for hearing care providers.
This presentation will provide an overview of changes that are currently happening in hearing healthcare and what we expect to come over the next few years. A particular focus will be given to AI, how the role of audiology will evolve as AI is integrated in hearing services, and ethical considerations in the use of AI in hearing healthcare. Research at NAL in a variety of these areas will be used to provide insight into understanding these changes and provide guidance on how hearing care professionals can manage this evolution.
Biography
Brent Edwards Ph.D. is the Director of the National Acoustic Laboratories, an Australian Federal Government centre for research on hearing loss, where he leads research and innovation initiatives that focus on transforming hearing healthcare. For over 20 years he headed research and technology at major hearing aid companies (GN ReSound, Starkey) and at Silicon Valley startups that developed innovative technologies and clinical tools used worldwide. Dr. Edwards founded and ran the Starkey Hearing Research Center in Berkeley, California that was a leading site for research in hearing impairment and cognition. Dr. Edwards is a Fellow of the Acoustical Society of America, a Fellow and current President of the International Collegium of Research Audiology, an Adjunct Professor at Macquarie University and at the University of Queensland.
Keynote Lecture: The ACHIEVE Trial in Perspective: What do audiologists need to know?
Dr Theresa Chisholm, Professor of Audiology & Vice Provost, University of South Florida
Abstract
The independent association of age-related hearing loss with cognitive decline highlights a need to understand the potential influences of hearing intervention (HI) on cognition. The Aging and Cognitive Health Evaluation in Elders (ACHIEVE) randomized controlled trial (Clinicaltrials.gov NCT03243422; NIH funded R01AG055426), was designed to determine the efficacy of best-practices HI versus a successful aging (SA) education control intervention on the 3-year trajectory of cognitive decline in older adults. 977 participants (70-84 y/o) with mild-moderate hearing loss and normal cognitive function were recruited: (a) from the cardiovascular health (Atherosclerosis Risk in Communities [ARIC]) observational study; or (b) de novo from the community. Intention-to-treat analysis revealed no difference as a function of intervention in the 3-year change in global cognitive decline. However, in a prespecified sensitivity analysis stratified by recruitment source, HI reduced 3-year cognitive change in the ARIC cohort by 48% compared to the SA control. While there was no difference as a function of intervention for the de novo cohort, they had fewer risk factors for and a slower rate of cognitive decline than the ARIC cohort. Additional analyses demonstrated HI improved communicative function, reduced cortical thinning, and positively impacted social health and well-being. Implications for audiological practice are discussed.
Biography
Dr. Theresa H. Chisolm is a Professor of Audiology in the Department of Communication Sciences & Disorders at the University of South Florida (USF) where she began in 1988 as an Assistant Professor. Dr. Chisolm specializes in rehabilitative audiology and is a licensed and certified audiologist, with over 40 years of clinical and research experience. Previous research examined the efficacy of a computer-based auditory training program for use post-hearing aid fitting, approaches to auditory rehabilitation for veterans with mild traumatic brain injury, and the outcomes of open-fit hearing aids. Her role in the ACHIEVE trial, as a co-investigator and USF site PI, spanned from initial conceptualization to development of the development of the manualized best-practices hearing intervention to implementation and fidelity monitoring with her co-PI colleagues at USF’s Audiology Rehabilitation Clinical Trial’s laboratory (ARCT), Drs. Victoria Sanchez and Michelle Arnold. Dr. Chisolm and the ARCT laboratory members are continuing their work on data analysis, interpretation and dissemination of the original ACHIEVE trial data and participating in several ongoing follow-up studies. In addition to her teaching, research and clinical work, Dr. Chisolm is currently serving in an administrative role as the Vice Provost for Strategic Planning, Performance & Accountability at USF.
Keynote Lecture: Managing the social and emotional wellbeing impacts of hearing loss: Interventions and approaches that can be implemented to augment current clinical practise
Dr Bec Bennett, Senior Research Audiologist, National Acoustic Laboratories, Australia
Abstract
Over the past decade, there has been an increased focus on the social and emotional well-being impacts of hearing loss. This presentation will highlight recent research in this area, helping delegates understand the profound effects hearing loss can have on individuals, including insights from the client perspective. We will discuss the current limitations within audiology practice in addressing these needs and explore various global approaches that audiologists use to better support the social and emotional well-being of their clients.
A key focus will be on the AIMER program, designed to enhance clinicians’ knowledge, skills, opportunities and motivation to support their clients’ well-being more effectively. Delegates will have access to specific resources developed for the AIMER program, which they can apply in their clinical practice.
We will also touch on how the five-step plan can be used to integrate social and emotional well-being support into existing audiological services. Finally, we’ll provide a sneak peek at a new educational health behaviour change mobile application being developed by the National Acoustics Laboratories. This app is designed to help new hearing aid users manage the social and emotional challenges associated with hearing loss.
Biography
Dr Bec Bennett is a Senior Research Audiologist at the National Acoustic Laboratories. Her research focuses on adult audiological rehabilitation, the social and emotional impacts of hearing loss, and eHealth service delivery. She recently led a research program co-developing a multifaceted behaviour change intervention to improve how hearing healthcare clinicians provide social and emotional support within the audiology context. She currently leads a program of work developing a digital self-management tool to address the social and emotional impacts of hearing loss. Bec is a 2022-27 NHMRC Investigator Fellow and a Director of the Board, Audiology Australia.
Keynote Lecture: Deaf awareness – are our services really accessible (title tbc)
Dr Sam Lear, Senior Audiology Policy Advisor at NDCS & Crystal Rolfe, Director of Strategy at RNID
Abstract
“We know there are gaps in the deaf awareness of health professionals, and this includes some audiologists. Not all audiology services are truly accessible and respectful of the deaf person. Deaf awareness training for healthcare professionals often covers only the basics such as communication tactics- this is important, but there is much more to deaf awareness than this.
This session aims to increase audiologists’ awareness of the issues facing our deaf service users and their families, particularly around accessibility. We aim to encourage better understanding of different perspectives of deafness beyond the medical model, and understanding of the impact of the language we use around deafness. You will hear directly from deaf people about their experiences.
Whether you work in paediatric or adult audiology, have been practising for 3 months or 30 years, we hope that this session will encourage you to reflect on your own practice and what could be tackled in your own services to improve accessibility and deaf awareness”.
Biographies
John Bamford Lecture: A new era in the treatment of genetic hearing loss-genomic therapies
Professor Manohar Bance, Professor of Otology and Skull Base Surgery

Abstract
Genetic hearing loss has long been recognised as a major cause of childhood hearing loss. Increasingly with the R67 panel in the NHS, we are using this testing to understand the causes of hearing loss. There are many pitfalls, and several surprises when this kind of hearing loss testing is adopted widely, and we are finding out more and more.
Also, with the advent of gene therapies it is more important than ever to diagnose early genetic hearing losses. In this talk, I will discuss our learnings from our genetic hearing loss clinic, as well as discuss my involvement as the chief investigator for the CHORD trial for genetic hearing loss due to OTOF gene variants, with the AAV1 treatment in conjunction with Regeneron, and our early results
Biography
Professor Bance is the inaugural Professor of Otology and Skull Base Surgery at the University of Cambridge, appointed in 2017. Prior to that, he was Professor and Chair, Division of Otolaryngology at Dalhousie University in Canada. He trained in Otolaryngology-Head and Neck Surgery in Toronto and UCLA, finishing his training in 1995. He was on Faculty at the University of Toronto in Otolaryngology-Head and Neck Surgery from 1996-2001, when he moved to Dalhousie University..
Professor Bance is a surgeon-scientist, and runs the SENSE lab as a surgeon-scientist in Cambridge, as well as clinical supervision of the Otology and Skull Base Fellows. Prof. Bance is the Chair of the British Cochlear Implant Group, and Past President of the Royal Society of Medicine Section of Otology.
He performed the first gene therapy for hearing loss outside of China in 2022, and is Chief Investigator for a hearing loss gene therapy trial, as well as running the Genetic Hearing Loss Clinic in Cambridge.
Occupational stress in UK Audiologists
Mr Ryan Phillips, Clinical Scientist, Betsi Cadwaladr University Health Board
Abstract
Occupational stress is known to have detrimental effects on health care professionals worldwide. This study aimed to address a research gap by investigating sources and levels of occupational stress in UK audiologists. A mixed-methods cross-sectional design and convenience sampling were utilised. The study used the Audiologist Occupational Stress Questionnaire and an audiological working practices questionnaire The research included 100 registered UK audiologists and revealed that over a third of participants reported experiencing moderate or higher levels of occupational stress. Paediatric audiologists and those with a high daily patient load reported significantly higher stress scores than other specialties and those seeing fewer patients per day. Identified sources of stress for UK audiologists included clinical demands and time constraints, staffing issues, leadership in the workplace, and equipment availability. Reported impacts of stress encompassed mental health issues, fatigue, social life disruptions, and physical health concerns. The findings provided insights into the sources and levels of occupational stress experienced by UK audiologists, supporting existing research in other countries. The identification of consistent stress themes across the literature underscores the need for targeted support and interventions to ensure the well-being of audiologists and to empower them in maintaining their pivotal role in health care.
Biography
Ryan Phillips is a Trainee Clinical Scientist in the North Wales Audiology Service, part of Betsi Cadwaladr University Health Board. Ryan has an academic background in psychology and prior to beginning his career in healthcare he was an Air Traffic Controller in the Royal Air Force. Working in such a highly stressful environment is what sparked his initial interests in stress research. He has a keen interest in research and innovation, all areas of audiology and the psychosocial impacts of hearing loss and related disorders. He has recently celebrated his first scientific publication, “Occupational Stress in UK Audiologists” which was published in the American Journal of Audiology in July 2024.
Looking after your own wellbeing – putting evidence into practice
Ms Beth-Anne Mancktelow, Audiology Head of Service, Norfolk & Norwich University Hospital
Abstract 
Wellbeing’ has been taken to mean almost anything. In this talk, we will explore the evidence-base for wellbeing at work and, most importantly, how you can apply this to yourself and to your teams. You can expect to hear about the levels of evidence and a reminder of how to critique the literature in this area; NICE guidelines and their relevance to the NHS workplace; the NHS People Promise and why this may be important for you, and the local leaders programmes delivered by NHS England. We will explore the principles of wellbeing and help you to apply these into every day working life.
Biography
Beth-Anne is the Head of Service for Audiology at the Norfolk and Norwich University Hospital. Prior to this, she held a role looking after staff wellbeing at the same Trust, and prior to that was the tinnitus lead at St George’s Hospital in London. Beth-Anne is particularly interested in evidence-based approaches as they apply to both the clinical and non-clinical aspects of her role.
Dementia and Hearing Loss
Professor Tom Dening, Professor of Dementia Research, Honorary Consultant in Old Age Psychiatry, University of Nottingham
Abstract 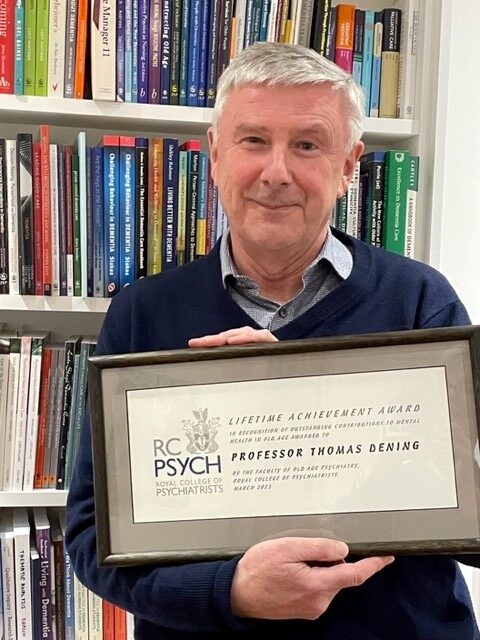
Recent evidence suggests that HL from middle age is an important potentially modifiable risk factor for dementia. There are various possible mechanisms; e.g. effects of increased cognitive load and sensory deprivation upon brain function and structure, or possible common causes like vascular disease. There may also be spurious associations from overdiagnosis of cognitive impairment among people with HL or vice versa (presumption that people with cognitive impairment are hearing-impaired). Thus, stating that HL causes dementia may be not wholly justified.
Can hearing interventions can prevent dementia? Most studies find lower rates of dementia in people with HL who wear hearing aids (HAs) versus those who do not. However, most studies are observational, so there may be other differences between HA users and non-users. The only large trial had mixed results, so the evidence is currently inconclusive.
The risk factor and prevention agenda has dominated recent dementia and HL research, but nonetheless many people will develop either or both conditions. Therefore, clinical aspects such as detection of cognitive impairment in audiology and hearing loss in memory assessment remain important, along with support and care of people with both conditions. Care home residents are likely to have both dementia and HL, and therefore more research about good practice in this area is needed.
This presentation ends by considering the development of a research agenda for dementia and hearing loss research, to put forward the most pressing questions for future attention.
Biography
Tom Dening is Professor of Dementia Research, University of Nottingham; and Honorary Consultant in Old Age Psychiatry, Nottinghamshire Healthcare NHS Foundation Trust.
Tom was appointed to his current post in 2012. His interests include a wide range of clinical topics and psychosocial aspects of dementia, and his main current research collaboration is around dementia and hearing conditions. He is one of the editors of the Oxford Textbook of Old Age Psychiatry, the leading international work in this field, 4th edition due in 2025. He is chair of the trustees of Trent Dementia Welcome – Trent Dementia – Helping people live well with dementia.
The Full Monty: stripping hearing back to health
Dr David Maidment, Senior Lecturer in Psychology & Lead Academic Tutor for Psychology, Loughborough University
Abstract 
Hearing loss in adults is associated with poorer health outcomes, such as depression, social isolation, cardiovascular disease, diabetes, and dementia, as well as negative health behaviours, including physical inactivity and malnutrition. Health behaviours have mostly been investigated as potential risk factors for the development of hearing loss and other chronic conditions, with little evidence on how positive health behaviours can be promoted in the population. Emerging evidence for an association between hearing loss and health concerns has resulted in a growing number of calls for researchers and healthcare professionals to consider the connection and balance between all aspects of an individual’s health, rather than focusing on individual health conditions in isolation. This presentation will outline how an integrative approach to health could be adopted by hearing healthcare professionals. It will be argued that audiology appointments may be a particularly effective time for clinicians to approach conversations about the adoption of positive health behaviours in adults with hearing loss. Such an approach aligns with the Making Every Contact Count (MECC) initiative, which aims to enable the delivery of consistent and concise health and wellbeing information to encourage individuals to engage in conversations about their health more generally.
Biography
David is currently a Senior Lecturer in Psychology within the School of Sport, Exercise & Health Sciences at Loughborough University. His research interests focus on interventions that aim to improve physical health and psychological wellbeing in adults with long-term conditions and disabilities, including hearing loss. David studied within the School of Psychology at Cardiff University, graduating in 2008 with a BSc in Applied Psychology. David then went on to complete an MSc (2009) and PhD (2013) at Cardiff. His PhD, funded by the Economic & Social Research Council, explored how different modes of speech interact in verbal short-term memory. David then went on to work as a Research Associate (2012-15) at the MRC Institute of Hearing Research, and a Research Fellow (2015-18) within the Hearing Loss theme at the NIHR Nottingham Biomedical Research Centre. In this latter post, David was involved in the development and evaluation of digital interventions for hearing loss, underpinned by contemporary models of health behaviour change
Differential patterns of auditory evoked potentials characterise tinnitus and hyperacusis
Dr William Sedley, Clinical Research Fellow and Consultant Neurologist, Newcastle University
Abstract 
Whilst tinnitus is defined by hearing sound with no external source, it is likely that this ‘phantom’ sound has its origins in the same mechanisms involved in the processing of external sounds. Tinnitus is also typically associated with hearing loss (its main risk factor) and hyperacusis (as least to a modest but significant degree). As well as these three interrelated factors, tinnitus often causes distress and alterations in attentional state (which itself affect sound processing). A final consideration is distinguishing changes in auditory processing due to the current presence of tinnitus itself from those facilitating its onset, maintaining its persistence, or mediated by the associated level of distress or altered attention.
Here, I present some of the substantial past and ongoing work by our and other groups to understand the multifaceted relationships between tinnitus and cortical evoked responses to sounds in humans. This will cover 40 Hz steady state responses (ASSR) as a marker of early primary cortical processing, N1-P2 (and its intensity dependence) as an indicator of later primary-nonprimary auditory cortex interactions (and serotonergic function), mismatch negativity (MMN) as a marker of pattern or prediction violation, and P300 as a marker of conscious reactions.
Biography
I am a medical graduate, combining clinical practice in neurology with research in clinical and basic neuroscience.
I graduated from Nottingham University in 2007, and have been working as a doctor and conducting research in Newcastle ever since, completing my PhD in 2015, and commencing my first NHS consultant post in 2021.
My group’s research focuses on high-level perceptual processing mechanisms in the brain, with a particular focus on hearing, and related disorders such as tinnitus and hyperacusis.
Our research is conducted on human volunteers, with and without clinical conditions, and uses a range of neuroimaging measures including EEG, MEG, fMRI and direct electrode recordings.
How some sounds get stuck: Key targets for change in misophonia
Jane Gregory, Clinical Psychologist, University of Oxford
Abstract
Misophonia is a relatively newly identified phenomenon of decreased tolerance to certain everyday sounds. It is distinguished from hyperacusis in that it is not the volume, but rather the pattern and meaning of the sounds, that contributes to the intense emotional, physical and behavioural reactions.
This presentation will provide an overview of misophonia from a psychological perspective, introducing a simple cognitive-behavioural model for understanding the distress and impairment caused by misophonia. A case example will be used to demonstrate how novel and safe experiences with sounds can lead to reduced intensity of reactions and improved functioning. There will be time for questions and discussion on how audiologists can support individuals with misophonia and when to refer on for psychological intervention.
Biography
Dr Jane Gregory is a clinical psychologist researching misophonia and the clinical lead for misophonia treatment at the Oxford Health Specialist Psychological Intervention Centre. She is co-author of the S-Five, a multidimensional questionnaire measuring key aspects of misophonia that can be used in research and to monitor change in clinical settings.
Dr Gregory’s research is driven by questions emerging from clinical practice, and she is currently testing whether misophonic behaviours are associated with changes in symptom severity and quality of life over time. Her misophonia research is funded by clinical academic grants from the Wellcome Trust and the National Institute for Health and Care Research (NIHR), which focus on research that can be immediately translated into changes in clinical practice.
She is the author of the self-help book, Sounds Like Misophonia: How to stop small noises from causing extreme reactions.
The Specialist Microtia & Atresia Clinic MDT
Marsha Jenkins, Principle Clinical Scientist (Audiology), St Thomas’ Hearing Implant Team
Mr Harry Powell, Consultant ENT Surgeon (Otology and Hearing Implants), Guy’s and St Thomas’ NHS Foundation Trust
Mr Simon Filson, Consultant Paediatric Plastic Surgeon, Evelina London (St Thomas’
Ms Sameera Miah-Moola, Clinical Lecturer & Maxillofacial Prosthetist, Clinical Lecturer & Maxillofacial Prosthetist, Kings College London & Guys Hospital
Abstract
Patients with microtia and aural atresia have a complex craniofacial condition that can impact on many aspects of their lives. It is essential that these patients and their families have access to specialised teams able to provide up to date information. A multidisciplinary approach should be taken to provide holistic, individualised assessments and interventions.
The St Thomas’ hearing implant team have been caring for patients with microtia and atresia for over 20 years and the Specialist Clinic was established in 2006. The multidisciplinary clinic includes ENT, Plastic Surgery, Maxillofacial, Prosthetic, and Cleft Palate consultants along with Audiological Scientists and Speech and Language Therapists from the Hearing Implant team. The clinic is for patients who have microtia and atresia who would like to explore hearing solutions, ear prosthetics and reconstruction. The clinic is held 4-5 times per year and offers virtual information sessions and in-person consultations. The Specialist Clinic enables patients and families to meet all specialists in one session rather than attend multiple appointments in several different departments, this enables optimal coordinated care for children and adults with this condition.
Members of the team from ENT, Plastics, Prosthetics and Hearing Implants will discuss the role they play in this multidisciplinary team and the benefits of joint working for patients and professionals.
Biographies
Marsha Jenkins
Marsha is joint Lead Clinical Scientist at the Paediatric Hearing Implant Centre at St Thomas’ Hospital, London. The centre offers all hearing implants and Marsha also co-ordinates the Bone Conduction & Middle Ear Implant Programme. She has over 20 years’ experience of working in the field, joining the team in 2001. She also co-ordinates The Specialist Microtia & Atresia Clinic, which is a multidisciplinary clinic involving ENT, Plastics, Prosthetics, Maxillo-facial and Audiological and Rehabilitation professionals.
Marsha has a B.Sc. (Hons) Biochemistry and an M.Sc. in Audiological Science. At the start of 2023 Marsha started a part-time PhD at the UCL Ear Institute which is exploring optimising outcomes for children with unilateral hearing loss.
Sameera Miah-Moola, MIMPT, is a Clinical Lecturer in Maxillofacial Prosthetics at Kings College London and Guys Hospital where she teaches on three international postgraduate programmes, after completing her MSc at Kings in 2017. She recently joined the KCL adacemic team after 6 years of post-qualification clinical pactice at Guys, compromising of the manufacture and delivery of various facial and body prosthetics and leading the representation of prosthetic options at the Specialist Microtia and Atresia Clinic.
At this years BAA conference, Sameera will be part of a panel sharing insights especially for those directly involved in the referral process for paediatric auricular prosthetics and her latest clinical experiences.
Harry Powell
Harry Powell is a UK ear, nose and throat Consultant providing NHS and private care to adults and children.
He was inspired into ENT as a medical student in London at the United Medical and Dental Schools of Guy’s and St Thomas’ (1997-2003). Two and a half years of otology, cochlear implants, neuro-otology and skull base surgery at the Royal National Throat, Nose and Ear Hospital cemented his subspecialist interests, which include hearing rehabilitation, otosclerosis and implantable auditory devices.
He was awarded the Graham Fraser Memorial Fellowship and two Royal College of Surgeons grants for advanced surgical training in ear surgery and auditory implantation in Sydney, Australia, where he developed an interest in endoscopic ear surgery.
Harry returned to Guy’s and St Thomas’ NHS Foundation Trust as the otology and auditory implant fellow and was subsequently appointed as an Otology consultant there in September 2016. He has a number of specific research interests and collaborations all aimed at treating ear disease and improving hearing.
S ameera Miah-Moola
ameera Miah-Moola
Sameera Miah-Moola, MIMPT, is a Clinical Lecturer in Maxillofacial Prosthetics at Kings College London and Guys Hospital, where she teaches on three international postgraduate programmes, after completing her MSc at Kings in 2017. She recently joined the KCL academic team after 6 years of post-qualification clinical practice at Guys, compromising of the manufacture and delivery of various facial and body prosthetics, and leading the representation of prosthetic options at the Specialist Microtia and Atresia Clinic.
At this year’s BAA conference, Sameera will be part of a panel sharing insights especially for those directly involved in the referral process for paediatric auricular prosthetics and her latest clinical experiences.
Simon Filsom

Simon Filson – paediatric plastic surgeon
Mr Simon Filson is a full time Consultant Paediatric Plastic Surgeon and Head of the Paediatric Plastic Surgery Department at the Evelina London (Guys and St Thomas’ Trust).
He graduated from the Faculty of Medicine of the Newcastle Upon Tyne University, with Merit and then trained as a surgeon in the North East of England until 2011, when he moved to “Rambam” Hospital in Haifa, Israel, a famous trauma centre. The majority of the workload involved the reconstruction of complex war injuries and burns from Syria, Israel and the Palestinian Territories. Due to his surgical work, patient care and junior doctor training, in 2014, he was recognised with the prestigious Excellence award, “Oved Mitztayen”. To further his specialisation he is also trained in all aspects of Paediatric Plastic Surgery on a year’s fellowship with some of the world leading children’s surgeons at the Sick Kids Hospital, Toronto. On returning to the UK he continued his sub-specialisation with a Microsurgical and Breast reconstruction Fellowship at Guys and St Thomas’ Hospitals.
He has particular interests in all Paediatric facial reconstruction ranging from autologous ear to facial palsy reconstruction. He also specialises in vascular malformations and upper limb/chest wall reconstruction. He is passionate about education and improving the care of all children and is the Lead for Education in the Surgical and Anaesthetic Directorate.
How is technology changing cochlear implant care?
Professor Helen Cullington, Clinical Scientist (Audiology), University of Southampton Auditory Implant Service
Abstract 
Almost all aspects of cochlear implant care can now be done remotely: tuning, rehabilitation and lifelong care. The patient still needs to travel to hospital for the operation, but robotic surgery advances mean a remote surgeon could plan and program the operation, leaving the robot to do it – with on-site supervision. There are apps for patients to manage their care at home, for example adjusting programs, finding a lost processor, testing hearing and speech perception, and checking equipment. Communication technology inclusivity has improved rapidly – with real-time captioning, AI speech enhancement, Bluetooth connectivity, captioning smart glasses etc.
People with cochlear implants can now do things that people with normal hearing cannot do. For example, use smartphone translation streamed directly to their implant – communicating in a multilingual environment with no visual sign of translation. They can stream audible map directions to their implant – walking around a new city like a local. AI is integrated into everything cochlear implants do – from predicted mapping levels to speech enhancement in noise.
Where does this leave the cochlear implant clinician? Are clinicians embracing the new technology, or are they reluctant to change? Are patients happy, and are they receiving the best experience and outcomes?
Biography
Helen is an audiologist and researcher at the University of Southampton Auditory Implant Service in the United Kingdom, and past Chair of the British Cochlear Implant Group. She is Editor-in-Chief of the Journal Cochlear Implants International. Helen is captivated by cochlear implants and the use of technology to improve people’s lives; much of her research has been focussed on remote care for people with implants. Helen has worked in cochlear implants for her whole career (more than 30 years) in six cochlear implant centres around the world.
The role of balance vigilance in chronic dizziness and vestibular disorders
Dr Toby Ellmers, Sir Henry Wellcome Fellow, Imperial College London
Abstract
Vigilant monitoring of balance has been proposed to underpin various chronic dizziness disorders, including persistent postural–perceptual dizziness (PPPD) and so-called ‘unexplained dizziness’ in older adults. This talk will precent recent experimental and clinical findings that support this proposal. Particular emphasis will be placed on presenting work that illustrates how such balance vigilance can (i) fundamentally alter the way that the brain processes vestibular and balance-related sensory information, (ii) disrupt and distort one’s perceptions about their level of postural (in)stability, and (iii) cause maladaptive changes in balance control strategies. The talk will culminate in the presentation of a new clinical outcome measure designed to assess a patient’s vigilance towards balance: The Balance Vigilance Questionnaire (Balance-VQ).
Biography
Dr. Toby Ellmers is a Sir Henry Wellcome Trust Fellow within the Centre for Vestibular Neurology (formerly Neuro-Otology Unit) at Imperial College London, under the mentorship of Prof Adolfo Bronstein. His research explores the psychological factors that affect balance, dizziness and vestibular function – with a particular emphasis on developing new methods of clinical assessment and management. The clinical outcome measures that he has developed have been translated into various languages and are currently being used in clinical sites around the world. He is a Co-Lead member of the World Falls Guidelines recommending body. In 2023, he was awarded the Promising Scientist Award from the International Society for Posture and Gait Research (ISPGR) for his work investigating how fear of falling affects fall-risk.
Persistent Postural Perceptual Dizziness
David Herdman, Clinical Academic Research Fellow, University College London & St George’s Hospital
Abstract
Persistent Postural-Perceptual Dizziness (PPPD) is a common and disabling condition characterised by persistent feelings of dizziness and unsteadiness. Dr. David Herdman will discuss what we currently understand about this disorder, including its pathophysiology, diagnostic criteria and treatment options. Dr Herdman will discuss why traditional vestibular rehabilitation may not always work for this population, and what we can learn from more cognitive-behavioural approaches to rehabilitation.
Biography
Dr David Herdman is the lead physiotherapist for the Neurology and Vestibular Physiotherapy Department at St George’s Hospital, London. He completed his PhD in Health Psychology from King’s College London and has recently started a post-doctoral Advanced Clinical Academic Fellowship from the NIHR, based at University College London (UCL) Queens Square. He has been Chair of the physiotherapy special interest group in vestibular rehabilitation (ACPIVR) and is the co-director of the UK vestibular rehabilitation competency accreditation. His current research interests include developing treatments for chronic dizziness/PPPD (the INVEST trial) and implementing evidence-based recommendations in emergency medicine to improve management of acute vertigo.
Unilateral deafness in children – evidence, challenges and experiences.
Dr Hannah Cooper, Lecturer in Audiology & Clinical Scientist (Audiology), UCL Ear Institute and Royal Berkshire NHS Foundation Trust
Abstract 
Unilateral deafness (UD) in children poses a challenge to parents and professionals. There are uncertainties about the impact of UD on a child’s development as well as a lack of clarity about the impact, either positive or negative, of interventions. Current guidance for management of children with UD is limited both in the UK and internationally. This translates to uncertainty for parents and professionals around management.
In this presentation we will explore the issues around UD and report on our body of research in this area. Firstly, the findings from a systematic review to evaluate whether hearing aids improve hearing/listening outcomes in children with permanent unilateral hearing loss will be presented. Secondly, we will report on the outcomes of a survey of paediatric audiologist practice for unilateral deafness in the UK and compare to a review of international practice. Finally, we will present the findings of a qualitative project to understand parent experiences of diagnosis and management of mild and unilateral deafness and develop information resources for families of children age 0-4 years.
Biography
Hannah Cooper is a lecturer in audiology at the UCL Ear Institute and a paediatric audiologist at the Royal Berkshire Hospital.
Using audit to give confidence in the provision of paediatric audiology
Mrs Catherine Magee, Enhanced Paediatric Audiologist, Northern Care Alliance NHS Group
Abstract 
The BAA quality standards for paediatric audiology provide us with an aspiration of excellent quality for us to work towards as paediatric audiologists. At first glance it’s very easy to think, yes we do that, that’s not an issue for us, we don’t do that fully but we meet most of what is outlined so that’ll do. However, have you checked that what you think happens is actually being delivered in clinical practice? When a hearing loss is identified and a decision to fit amplification is made, are 95% of children offered an appointment to fit the hearing aids within four weeks for permanent hearing loss? What about temporary losses? (Standard 1A6) Have you checked recently?
In this presentation, I will share how we at the Northern Care Alliance, used the paediatric quality standards to benchmark what we thought we delivered and then used vertical and horizontal audits mapped to the standards, to check exactly what was being delivered. The results highlighted some good practice but also areas for improvement and good learning opportunities. I will also touch on how you can use audit to look back through a cohort of data to show if ABR results marry the behavioural and PTA results, highlighting potential learning needs within the paediatric team.
Biography
I have been an NHS audiologist for 21 years, working in routine, complex, and highly complex testing, paediatric hearing aids and ABR assessments, albeit not all simultaneously. Interspersed with this, I spent 12 years managing a team of newborn hearing screeners, which provided me with valuable leadership experience. I am currently an enhanced paediatric audiologist at the Northern Care Alliance responsible for delivery of an audiology-led aetiology pathway. I am also a development and evaluation manager within the screening sub directorate of NHS England, working at a national level to oversee NHSP and other newborn screening programmes. I am passionate about making the journey for the child and family through screening, diagnosis and intervention as good as it can possibly be, to enable the children we identify to have the life opportunities they rightfully deserve.
Starting from Zero – A first steps in Quality Management toolkit
Mr Craig Tilt, Audiology Project Facilitator, Nottingham University Hospitals NHS Trust
Mrs Jenny Richardson, Chief Audiologist, United Lincolnshire Hospitals NHS Trust
Abstracts
Craig – Over the past year, there has been increased pressure on Audiology services to step up their quality assurance processes, and in some places to consider whether they can begin the IQIPS accreditation journey. Knowing how and where to start can feel overwhelming, particularly while continuing to deliver a clinical service. Based on feedback from services just starting their quality management systems, a toolkit has been developed to give people a jump-start. Based on processes used with
in Nottingham University Hospital NHS Trust for several years, the tool kit provides guidance on getting your document control process started and how that in turn supports building your audit plan and non-conformity system (CAPA). The session will give you a guided tour of the tool-kit, which includes templates, worked examples, how-to guides and accompanying documentation. One of the departments we worked with will described how they used the toolkit – and whether it worked. At the end of the session you will be given access to the whole tool-kit to download, so you can begin to use it on Monday.
Jenny – After much discussion amongst the team, we have been puzzled and petered by how to tackle audits and all things quality management following the Lothian investigations and subsequent Paed QS work. I was put in contact with Craig who very kindly shared some of the tools that he has been developing and asked to test them out and to offer some feedback.
petered by how to tackle audits and all things quality management following the Lothian investigations and subsequent Paed QS work. I was put in contact with Craig who very kindly shared some of the tools that he has been developing and asked to test them out and to offer some feedback.
My presentation is our experience of the struggles we have had on our quality improvement journey, using the tools that Craig has developed and how they have impacted out quality monitoring work as we are moving forwards to a position where we can consider IQIPs accreditation.
Biography
Craig Tilt has a background in process development and implementation. Working within Audiology at NUH since 2021, he has supported the development of the department’s quality management systems and retention of IQIPs accreditation through multiple assessments.
He doesn’t like piña coladas but does enjoy being caught in the rain.
Jenny is a Chief Audiologist at United Lincolnshire Hospitals. I begun my Audiology career with ULHT as a student and have worked hard to make it to the dizzying heights of Chief Audiologist.
I am the Head of Adult and Diagnostic Audiology for the department. I specialise in Vestibular testing and work hard to support the diagnostic testing for NHSP at our two main hospital sites. I can occasionally be found in theatre using my diagnostic skills to test complex patients and will happily get stuck in with the day-to-day Audiology when it is needed.
As well as my clinical case load, I am responsible for the operational management of our Boston site where I have line manager responsibilities for a number of staff. I am also the department’s Patient Experience Champion.
I am working towards my STPe and I am eager to support others on their journey into Audiology. I have worked with the BAA’s Regional Groups and with the Pub’s and Com’s Teams and I am passionate about raising the profile of Clinical Sciences and Audiology through education and training
Growing and maintaining the workforce. Feedback from placements and opportunities for development (how to make trainees happy and want to stay)!
Dr Ruth Vickerstaff. BAA Education Committee Member and Chair of the BAA Work-based Learning Sub Group
Abstract
Good quality work-based learning enables individuals to become the well-rounded professionals with the right skills and knowledge to provide safe and compassionate care of the highest quality. The aim was to understand the experience of Audiology students and create a set of recommendations that departments could implement.
Current students or recent graduates across pre-degree, degree, and post-graduate entry programmes in England, Wales and Scotland were interviewed about their experience. Northern Irish students were included but did not respond to invitations.
Students reported positive experiences when there was team psychological safety within the department, they had good relationships with their supervisor, and had a range of different opportunities. Students felt they would benefit from having training sessions with longer appointment times to allow them to work at a slower pace and to hear feedback in a timely manner.
Every student that had a good experience wanted to continue working in that department, those with a bad experience wanted to leave. Having a supportive culture is essential to delivering good quality education, and subsequent positive impact on the clinical skills of the student and therefore patient care and experience.
This presentation will share the findings from this study.
Biography
Ruth is presenting on behalf of the Work-based learning sub-group of the Education committee of BAA. The work-based learning group focuses on learning conducted in the work-place on any programme of study, e.g. apprenticeships, Practitioner Training Programme and Scientist Training Programme. The group takes a holistic approach to supporting services to deliver work-based learning, ranging from gathering feedback from students about their experiences of work-based learning to lists of questions you can ask a potential apprentice training provider. The group aims to deliver work that can be used directly by services. The membership consists of Audiologists (currently only NHS services, but welcome to non-NHS too), education providers, and manufacturer. If you are interested in joining this group please contact admin@baaudiology.org.
How to change the culture of your team – Leadership, change management, influencing
Laura Turton, Audiology Head of Service, NHS Tayside
Abstract
For the last 3 years Laura has been leading her team to successfully pass IQIPS in Scotland. Through this process the importance of shifting the culture of a team to succeed in change management has been highlighted as the key to success. The talk will cover:
- What culture is and how it affects the workplace
- Getting a grip on what your current culture is
- How to move from “we have always done things this way” to creating a culture which reflects your team’s vision
- The fear of change
- Change management in tough times
- Who can influence change and disrupt it
- Practical ways to influence
Biography
Laura has worked in NHS Audiology for over 20 years. She is currently Head of Audiology in NHS Tayside having relocated to Scotland 3 years ago. Her areas of special interest are providing a quality service and evidencing this, change management, writing practice guidance, and person-centred care. Clinically she sees people with hyperacusis, tinnitus and severe and profound hearing loss and enjoys all aspects of adult hearing rehabilitation.
In 2023 Laura was elected as a board member for BAA and has led the Professional Development committee for the last year.
The following speakers have been invited to present a paper from their abstract submission.
Achieving sound results: developing tailored physical activity interventions for adults with hearing loss
Dr Maria Goodwin, Postdoctoral Researcher, School of Psychology, Aston University
Introduction: Hearing loss in older adults is an independent risk factor for developing chronic health conditions (e.g., diabetes, cardiovascular diseases, and dementia). Physical activity is a modifiable behaviour that can reduce the risk of developing many chronic health conditions. Our previous qualitative research identified hearing loss specific barriers to physical activity, as well as theoretically and empirically derived intervention strategies that could be implemented to support physical activity in this population. To further this work, we aimed to explore the acceptability of these proposed intervention strategies.
Methods: A mixed-methods approach was taken. First, qualitative semi-structured interviews were conducted with four participants to explore perceptions of the interventions in depth. Responses were also used to refine questions and clarify explanations of the strategies. Second, a mixed-methods survey of adults 45-years and older was completed. Participants were asked to rate each of the strategies in terms of importance to them, with additional open-text questions to further explore why the most and least important strategies were selected.
Results: Strategies that support autonomy, such as information provision, were perceived most favourably (e.g., provided with information about the benefits of physical activity to hearing health). Participants also raised several potential barriers to the implementation of the proposed strategies, including who should communicate health information (e.g., “It should be a much wider consultation, but that then I suppose gets into an issue whereby, are audiologists trained or motivated to do that”).
Discussion: Taken together, less intrusive and prescriptive intervention strategies like information provision were preferred by participants. Yet research has shown providing information on personal risks and the benefits of physical activity only has small, short-term improvements on activity levels. Further co-design research is necessary to marry the discrepancies between strategies perceived as acceptable by those with hearing loss, and strategies identified as effective by research.
Biography
The experience of caregiver burden: A qualitative study of the experiences of friends and family of people living with hearing loss
Dr Georgina Burns-O’Connell, Research and Teaching Associate, Aston University
Hearing loss can significantly impact on daily life, not only for those who experience it but also for their family and friends who often become caregivers. While providing emotional and practical support is essential, it can also lead to caregiver burden. Given that hearing loss becomes more common with age, caregivers play an increasingly important role. This study aimed to explore the lived experiences and potential challenges faced by caregivers of people with hearing loss.
This is a piece of work within a larger study. The Hearing Loss and Patient Reported Experience (HeLP) study is a National Institute of Health Research Health Service and Delivery Research funded programme in the NHS in the UK (grant no NIHR 131597), sponsored by University Hospitals Bristol and Weston NHS Trust and delivered with Aston University and the University of Bristol.
Methods. In-depth interviews were conducted with a diverse group of caregivers, including parents of children with hearing loss, partners, and adults caring for ageing parents. The interviews were analysed using constant comparative methods and reflexive thematic analysis to identify patterns and understand the varying levels of caregiver burden.
Discussion. The analysis showed that different levels of caregiver burden were experienced across the lifecourse, and identified the factors that influenced this variation. The study highlights the emotional and practical demands on caregivers.
Conclusion. In illustrating the potentially significant burden experienced by caregivers of people with hearing loss, an understanding of how their support can be harnessed can be developed. This could lead to caregiver challenges being mitigated and in turn, improving the experience of living with hearing loss.
The Music Audiometer: Can we use music stimuli to test hearing in children with social and communication disorders?
Bradford Backus, Managing Director, Audio3 Ltd
Abstract
Since 2016, about 1 in 3 preschool-age children arriving at the Chear clinic did not respond to warble-tones (WT) or narrowband-noise (NBN) well enough to complete a traditional hearing assessment. Although the median age for establishing single frequency hearing response in SCD cases is 3 years, in some cases testing may continue into the teenage years (Bonino 2023). Bonino concludes: “Results reflect a failure in our methods— not in the child. We need new behavioural assessments and an informed strategy”.
Method: The NHS Paediatric Clinic at Guys and St Thomas’s, Chear Ltd, London Southbank University and Audio3 Ltd have collaborated to develop a novel ‘Music Audiometer’ with grant funding from Innovate UK. The research includes creating hardware/software, determining frequency bandwidths required to maintain recognition of familiar songs, ensuring sound-field calibration, and developing a new type of audiogram for displaying music response levels (mRLs)—which are different than those for pure-tone detection.
Results: A feasibility study of 30 cases is described. We show that music audiometry can succeed where WT or NBN stimuli fail. In addition, we find that while current advice is to use music only to condition children toward doing traditional WT or NBN tasks, many children never ‘graduate’ to these traditional stimuli—so developing a useable music-based hearing threshold is needed.
Conclusion: Music can be used as a test stimulus. The best way to do this is still unknown. Our aim is to establish new clinical equipment/protocols that can use music as a stimulus— ones that are feasible, practical and accurate. Our collaboration between clinicians, academics, and innovative companies shows how working together can produce new audiology techniques.
Biography
Bradford Backus MIT PhD – Managing Director at Audio3 Ltd. Bradford holds degrees in electrical engineering and psychoacoustics and did post-doctoral work at UCL in otoacoustics emissions with Prof. David Kemp. Since that time, Bradford has worked to translate all this science into products that help people hear better. He has worked for: Otodynamics–developing their low noise EABR systems, Oticon Medical’s CI division–where he authored 19 patents, and now is a consultant for Cochlear Corp.
Enacting Informed Choice: Investigating parental experiences of receiving support and information in relation to language and communication options, and the influences and impact on their abilities and opportunities for informed decision making in Scotland.
Gwen Carr, Independent Consultant, on behalf of NDCS
Abstract
Creating an environment in which families receive full, unbiased information and have access to the support and experiences they need in order to explore and understand what different communication and language choices may mean for them and their child is a key aspect of quality and effective early support. Undertaken on behalf of the UK National Deaf Children’s Society, and supported by NHS Scotland’s Hearing Impairment Network for Children and Young People (HINCYP), this project investigated the context for supporting and enacting parental informed decision making in Scotland.
The project addressed 4 key areas: Parental reflections on the information and advice received from professionals about language and communication; the contexts in which families receive information and how these affect their attitudes, feelings and decisions; parental perceptions of how specific messages, practices or professionals impacted their decision making, identifying factors which were helpful, empowering or influential or conversely, less helpful, restrictive or discouraging; and the implications of families’ experiences for professional practice and communication with families.
Data were collected via a desktop review of publicly available information relating to Informed Choice in language and communication in the Scottish context, an online questionnaire in both English and BSL for parents, in depth interviews with parents, and online informal focus groups and telephone interview with professionals across the full care pathway.
From both professional and parental perspectives, barriers and constraints as well as enablers and opportunities for ensuring an environment in which families can make informed decisions about language and communication, were identified, with implications for both professional practice across the care pathway and for the systems in which information and advice is shared. This presentation will give an overview of the project’s key findings and recommendations for service development in relation to enabling informed decision making for language and communication for families.
Biography
Gwen Carr is a Consultant in Early Hearing Detection and Intervention (EHDI) and Honorary Lecturer at the UCL Ear Institute. Previously Head of Local Authority Sensory Support Services and subsequently Director of Services / Deputy CEO at NDCS, she went on to be Deputy Director of the NHS England NHSP and then National Programmes Lead for antenatal and newborn screening for Public Health England. Following retirement, Gwen now works in EHDI research, training, and service development, and serves as a member of several advisory boards and research groups related to childhood deafness and parent support both nationally and internationally .
Revealing the struggle for silence: highlighting the mental health crisis in people living with tinnitus
Nic Wray, PhD student, NIHR Nottingham Biomedical Research Centre, University of Nottingham
Abstract
Tinnitus UK wished to examine the experiences of people living with tinnitus (PWT) who accessed healthcare support for the condition.
Method. An online survey was conducted in December 2023, publicised via Tinnitus UK’s social media and newsletters.
Results
The impact of tinnitus on quality of life and mental health can be severe.
Over 1 in 5 of PWT surveyed had had thoughts of suicide or harming themselves in the last year.
More than 8 out of 10 respondents experienced low mood or anxiety in the last year, with 7 out of 10 feeling hopeless or helpless.
Sleep disturbances affect 85.7% of respondents.
The emotional impact of tinnitus is significant, with 68.4% reporting low self-esteem and 54.9% struggling to think rationally.
Tinnitus is linked to social isolation, impacting relationships and daily life.
Access to healthcare. Half of respondents obtained GP appointments within a week, but 16% waited over a month. Referrals to secondary care decreased to 57.9% (2020: 64%), with 11.7% not offered a referral.
There is limited mental health support from GPs, with only 5% offered Cognitive Behavioural Therapy (CBT) as recommended in the NICE guidelines.
Reports of waiting more than 12 months for a secondary care appointment has tripled from 2019 to 2023, with 1 in 6 facing waits of more than a year.
The increase in waiting times for audiology appointments impacted quality of life for two thirds of respondents.
Discussion. Our survey starkly revealed the substantial toll tinnitus can take on mental health, emphasising the urgent need for comprehensive support and intervention measures to address the psychological challenges associated with this condition.
These findings underscore the imperative for enhancements in the initial stages of tinnitus care, including timely access to appointments, improved reassurance, increased dissemination of information by healthcare professionals and increased access to psychological support.
Biography 
Nic Wray is a PhD student at the University of Nottingham NIHR Nottingham Biomedical Research Centre, having previously worked as Tinnitus UK’s Communications Manager for over 14 years. They are an award-winning health information author on tinnitus.
Their main interest is the lived experiences of people with tinnitus and hyperacusis. They are passionate about communicating both research findings and personal stories about the conditions to help people improve their health and quality of life.
An evaluation of the prevalence of mental health conditions in patients seen in the Tinnitus Clinic and the access to Psychology Service
Alexandra Lusty, Specialist Audiologist, CUH NHS Foundation Trust
Abstract
Co-morbidity of Tinnitus and anxiety and/or depression is well documented and NICE guidance advocates Psychological therapies for tinnitus related distress remaining after tinnitus support has been given, initially in the form of group or digitally delivered CBT. The service needs of Psychology support for the Tinnitus Clinic were evaluated.
Objectives: To evaluate the prevalence of significant mental health concerns in the population and to understand what Psychological Therapies our patients are currently able to access.
Methods: The clinical notes of all adult patients seen in the Tinnitus Clinic between December 2020 were reviewed. Hospital Anxiety and Depression scores and whether Mental Health support was documented in their Individual Management Plan (IMP) was recorded. Where access to Psychological therapies was included in IMPs, a questionnaire looking at service access was sent. Subsequent clinical notes were examined for documentation of whether services had been accessed.
Results: Prevalence of significant anxiety and/or depression was consistent with previously published data at 26%. 31% of patients who were recommended Psychological therapies were able to access support, mainly individually delivered CBT. 48% did not pursue selfreferral to local IAPT services.
Discussion: There are barriers to access of Psychological therapies as part of Tinnitus management, which may include patient education, societal stigma, and technology barriers. Delivery of Psychological therapies in our area is not consistent with NICE recommendations.
Conclusion: There is a clear service need for Psychological therapies for Tinnitus Service users but at present, only around 1/3 of those who may benefit are accessing support. When support is accessed, it is not in the form recommended by NICE guidelines. Further service evaluation and development work is indicated to understand the barriers to access and explore provision of Tinnitus focused CBT delivered digitally or through group sessions.
Biography 
Aly is a Specialist Audiologist working at Addenbrooke’s Hospital. She works across the Tinnitus and Paediatric teams and leads the Paediatric Tinnitus service.
The UK National Registry of Hearing Implants (NRHI) – Improving patient safety and outcomes
Jenny Townsend, Principal Clinical Scientist, Betsi Cadwaladr University Health Board
Katherine Wilson, Lead Clinical Scientist, St Thomas’ Hearing Implant Centre
Abstract
There are over 22,000 cochlear implant users in the UK, but no national coordinated feedback loop to evidence that these devices are safe and effective. In order to address this and respond to the findings of the Cumberlege report, the British Cochlear Implant Group initiated a steering group to develop a national registry.
Methods: a National Registry has now been set up under the NHSE Outcome Registries Programme, and is being piloted in 5 centres. The initial scope encompasses cochlear implants; national roll out to all CI centres is planned for 2025. A dataset for bone conduction hearing implants is in development; all centres providing BCHI will be required to input data to the NRHI in due course.
Results: An update on the progress towards NRHI development and roll-out will be presented.
Conclusion: All types of hearing implants (including BCHI, MEI, CI and ABI) will be recorded in the NRHI in future. This will ensure improved safety and outcomes for patients, to meet requirements of the Medicines and Medical Devices Bill 2021.
Biographies
Jenny Townsend AuD MSc CS06598 AHCS HSS Register 
I have worked in North Wales audiology for the last 25 years and in the CI service for 20 years, leading the hearing implant service since 2015. My current activities include being local PI for the INSPIRE (CI remote care) study and involvement in development of a national device registry for hearing implants, seconded 0.1WTE to NHSE as part of the Audiology ORP clinical steering board.
Katherine Wilson 
Katherine has worked at St Thomas’ Hospital in the field of hearing implants for the past 24 years. She has been a Trustee to the British Cochlear Implant Group (2017-2023), National Chair for Hearing Implant co-ordinators (2012-2021), and has sat on multiple Advisory Boards for Hearing Implant Manufacturers. Katherine helped establish the London Paediatric ABI Centre, and in 2019 her team won the NHS Health Hero Award in the Ground-breaking Pioneer category. Katherine programmed the youngest baby (3 mos) to be implanted in the UK, appeared in various media programmes about hearing implants, sits on the NHSE Oversight Registry Board and chairs the National Registry Steering group to develop a UK-wide Hearing Implant Registry.
Cochlear Implants in Children with Partial Hearing: Data from a 10-year UK collaboration
Marette Ambler, Principal Clinical Scientist (Audiology), Midland’s Hearing Implant Programme
Katherine Wilson, Lead Clinical Scientist, St Thomas’ Hearing Implant Centre
Abstract
Introduction: Simultaneous bilateral cochlear implantation is now the recommended treatment for children with partial hearing. For the past 10 years two paediatric hearing implant programmes in the UK have worked in a unique collaboration, sharing and defining our practice, monitoring outcomes, collating our joint data, and presenting and publishing our work with children who have partial hearing. The hearing preservation surgery technique has been used successfully for all children with functional low frequency hearing (i.e. ≤65dBHL at one or more low/mid frequencies). We will present our experiences and outcomes with this group.
Methods: We defined Partial Hearing as having pre-operative hearing thresholds of ≤65dBHL at one or more low/mid frequencies. We have monitored a range of outcomes with this group including preservation of hearing at activation, use of electro-acoustic stimulation (EAS), long-term hearing preservation, functional outcomes and quality of life.
Results: Data will be shared on 140 paediatric patients (210 ears) who form this cohort. 92% of cases have complete or partial preservation of hearing. Cochlear implants (CIs) outperform the child’s hearing aids in all patients with improvements in listening, language and quality of life, irrespective of the level of preservation, the surgery type or the device used.
Conclusion: Hearing preservation electrodes and surgical techniques, alongside EAS, has made CIs more accessible to this group of children. Through the unique collaboration between our two teams, we have demonstrated excellent rates of hearing preservation in a large group of children with partial hearing. However, for this group of children, the real issues are those in relation to speech & language development, academic achievement and quality of life.
Our collaboration has allowed us to shape our multidisciplinary team assessment, refine our counselling and demonstrate extremely positive functional outcomes to our patients who can be confident in our recommendations and clinical practice.
Biographies
Marette Ambler
Katherine Wilson 
Katherine has worked at St Thomas’ Hospital in the field of hearing implants for the past 24 years. She has been a Trustee to the British Cochlear Implant Group (2017-2023), National Chair for Hearing Implant co-ordinators (2012-2021), and has sat on multiple Advisory Boards for Hearing Implant Manufacturers. Katherine helped establish the London Paediatric ABI Centre, and in 2019 her team won the NHS Health Hero Award in the Ground-breaking Pioneer category. Katherine programmed the youngest baby (3 mos) to be implanted in the UK, appeared in various media programmes about hearing implants, sits on the NHSE Oversight Registry Board and chairs the National Registry Steering group to develop a UK-wide Hearing Implant Registry.
Measuring Patient Experience Alongside Patient Outcome. The NIHR’s Hearing Loss and Patient Reported Experience study
Dr Helen Pryce, Reader in Audiology, Aston University
Abstract
This presentation will share findings from the Health and Social Care Delivery research funded Hearing loss and Patient reported Experience study (NIHR 131597). We will share the development of a model of how people experience hearing loss and what affects that experience.
The model underpins the new Patient Reported Experience Measure in Audiology. This measure has been developed using factor analysis and RASCH modelling to identify critical items to ask. The new PREM is now available free of charge to all audiology providers and will enable compliance with NHS England’s requirements to measure both patient outcome and patient experience.
Our presentation will describe the qualitative and quantitative research processes, survey results from a sample of 401 participants and detailed PPIE and stakeholder engagement.
Biography 
Dr Helen Pryce is a Reader in Audiology and Hearing Therapy at Aston University and Senior Hearing Therapist at HCRG Care Group. Helen has been in clinical practice since 1990 and has subsequently researched rehabilitative aspects of audiology, including leading the developments of decision aids in UK audiology, identifying mechanisms to explain variation in patient experience and outcome. Helen is the Programme Director for the Hearing Therapy Programmes at Aston and has taught at several UK universities. Helen is the Chief Investigator for the NIHR’s Hearing Loss and Patient Reported Experience study.
‘The burden is very much on yourself’: A qualitative study to understand the illness and treatment burden of hearing loss across the life course
Sian Lickess, Research Associate, Aston University
Abstract
Objectives: There is growing recognition of the illness and treatment-related work that patients must do to manage chronic illness alongside daily life demands. This presentation will share qualitative findings from the Health and Social Care Delivery research funded Hearing loss and Patient Reported Experience (HeLP) study. This work sought to understand the burdens of illness (e.g., coping with hearing loss in daily life) and burdens of treatment (e.g., seeking help and using interventions) experienced by people living with hearing loss across the life course, and the resources they draw upon to manage the workload.
Methods: Forty-six participants aged between 16 and 96 years recruited through audiology services, and non-clinical services (e.g., lip-reading classes) participated in semi-structured interviews. Data were analysed thematically and informed by May et al.’s (2014) burden of treatment theory to understand how participants described the “work” of living with hearing loss and the resources they drew upon to ease the burdens.
Results: Participants faced the burden of illness by working to understand their hearing loss, managing emotional responses to changes in sound, social interactions, and identity, and coping with daily communication frustrations. The treatment burden was marked by feelings of abandonment and uncertainty; participants had to emotionally adjust to hearing technology and deal with the unpredictability of their hearing progression. To alleviate these burdens, they relied on internal resources (resilience, health literacy, cognitive abilities) and external resources (social support, financial means, information, and technology).
Conclusions: Managing hearing loss demands considerable effort, encompassing practical, psychosocial, and relational tasks that often fall on the individual and remain unseen. Recognizing the hidden workload experienced by individuals with hearing loss is crucial. Expanding approaches in audiological care, such as lifeworld-led care and family-centred care, could enhance patient capacity and reduce the burden.
Biography 
Dr Sian Lickess is a Research Associate at Aston University and curently working with colleagues on the Hearing Loss and Patient Experience (HeLP) study – an NIHR Health Services and Delivery Research grant which seeks to develop the first Patient Reported Experience Measure (PREM) for people with hearing loss. Sian is a Chartered Psychologist with the British Psychological Society (BPS) and is particularly interested in exploring the social and emotional impacts of hearing loss. She has expertise in qualitative research, health literacy and the development and evaluation of psychosocial interventions.
Thursday 15:15 – 15:45: MRI compatibility in active bone conduction implants – ensuring patient access to essential imaging – Dr. Anne Small, Clinical Research Manager, Cochlear
Friday 09:50 – 10:20: Driving Change in Audiology: Influencing Pathways for Better Patient Care – Ruth Thomsen, Scientific Director, NHS England
Thursday 14:45 – 15:15: Clinical Leadership – Ruth Thomsen, London Regional Lead HCS & Clinical Director for Physiological Sciences and SRO for Children’s Ear Checks
Biography
Having worked in Audiology for over 40 years in NHS, Education & training and R&D, I am at my happiest when with my clan!
I stepped into a Clinical Leadership role following a Clinical Fellowship with responsibility for over 54 Healthcare Scientific Professions
I was ‘NHS Inspirational Leader of the year’ in 2019, ‘Inspiring the future leaders’ award in 2020 and the NASEN leadership award in 2024 for the coproduction of the ear checks program. And also made an honorary Fellow of the Academy for HCS after receiving the President’s award for her role in developing HCS Leadership, the leadership Journal and establishing a HCS Leadership faculty.
My role is always changing, but currently I am working in diagnostics, virtual wards, med tech and supporting the Office of the Chief Scientific Officer in leadership development, Clinical Engineering and Audiology and the ear check program. With a constant eye on accreditation and quality, innovation spread and adoption, I believe is what scientists can do best. I enable professional diversity by working collaboratively and I am a great fan of co-production as an enabler to working across complex health and care systems at a National, Regional and Local level.
Friday 11:55 – 12:25: Auracast – Dr Megan Quilter, Lead Audiologist, GN Hearing
Join Interacoustics during their presentations at BAA conference 2024
Thursday 12:10 -12:40: Helping you to work smarter, not harder: innovations in diagnostic and rehabilitative technology to support Audiology – Jack Bennett Clinical Training Manager Interacoustics UK
Jack will discuss examples of the new technology available to Audiologists which support their clinics in ways that reduce time-consuming processes, allowing them to do the most important things, like counselling their patients. He will cover Auto-REMs, Automated hearing tests, Quality Assurances tools and more.
Thursday 16:15 -16:45: Introducing the new Aided Cortical “ManU-IRU” stimuli – Anisa Visram PhD, Lecturer in Audiology, Manchester University
Anisa will discuss the development of the ManU-IRU stimuli and how aided cortical testing can be introduced into clinical practice.
Thursday 11.40am – 12.10pm: “Using Speech Audibility for Clinical Decision Making in Paediatric Audiology”
Ryan McCreery PhD Vice President, Research, Boys Town National research Hospital
Ryan McCreery is the Vice President of Research and Director of the Audibility, Perception, and Cognition Laboratory at Boys Town National Research Hospital in Omaha, Nebraska, USA. Ryan’s research seeks to develop strategies to optimize outcomes for children with hearing loss who use hearing aids. Ryan received the Early Career Contributions to Research award from the American Speech Language Hearing Association in 2013 and was named ASHA Fellow in 2020.
Abstract:
Speech audibility is the proportion of a speech signal that a person can hear in a given listening situation. Our research over the past 10 years has revealed that a child’s access to the acoustic cues that comprise spoken language is a powerful predictor of auditory, language, cognitive and academic outcomes in children who wear hearing aids. In this presentation, applications of speech audibility to support clinical decision making will be discussed, including using unaided audibility to support hearing aid candidacy decision for children with mild bilateral or unilateral hearing loss. The use of measures of aided speech audibility as an outcome measure that can be used to inform decisions about modifying intervention for children who use hearing aids will also be highlighted. Audibility-based counselling tools that audiologists can use to support children with hearing loss and their families will also be shared.
Friday 9.20am – 9.50am: “Counseling Patients to Support their Hearing Health Literacy”
Dave Gordey, AUD (C), Ph.D. Director of Pediatric Audiology and Research, Oticon Denmark
Dave Gordey, Ph.D., has been a pediatric audiologist for over twenty-five years. Dave is the director of pediatric audiology and research at Oticon Global headquarters in Denmark. Dave is an adjunct professor at Western University and Salus University. Dave’s current research projects include pediatric hearing aids, counseling, functional communication deficits in children with normal peripheral hearing, and the social and emotional development of children with hearing loss.
Abstract
Patient health literacy is described as the ability for an individual to obtain, process, and understand, information provided to them by their hearing health-care professional and feel they can make decisions based upon that information. The quality of an audiologist’s communication skills has a direct impact on a patient or parent’s understanding of hearing loss and adherence to recommendations for use of hearing technology. Recent research has suggested that the audiogram may not be meaningful for patients and parents as a tool to support their understanding of hearing loss.
A qualitative study using interview research was completed with participants being asked to reflect upon their experience with their audiologist and the informational counselling that was provided. Findings from this study will be shared with conference participants.
Learning Objectives
- Describe the key components of Self-Determination Theory.
- Describe factors that support informational counselling for patients and parents.
- List the resources patients and families want most from their audiologist.
Thursday 14:15 – 14:45: It’s time to talk about hearing – Gordon Harrison, Specsavers Director of Audiology and Professor Kevin Munro
Friday 12:25 – 12:55: Quality standards: a workplace revolution – Gordon Harrison, Sonam Sehemby and Chris Lakin, Specsavers
With thanks to our Official Conference Sponsors

